Imaging 2020: A Closer Look
When we talk about injuries, we often hear of primary care physicians and orthopedic specialists performing imaging in order to assist patients in treating musculoskeletal pain.
Imaging can include, but is not limited to, MRIs, X-rays, or CT scans. Although these tests may help feed our curiosity to “look under the hood,” they may not always be the best place to start.
Balancing Healthcare Costs and Imaging
In a world today looking to decrease healthcare costs, imaging can be a large line item: a study done by Parker et al estimates that musculoskeletal imaging costs are projected to reach $3.6 billion dollars in 2020. While the cost might be worth the peace of mind brought by the imaging results, studies have found that imaging does not actually ease fear and worry about the cause of pain.
Once being labeled with “degenerative disc disease” or “knee arthritis,” patients tend to define themselves in terms of these issues.
Are Abnormal Findings Always Relevant?
Additionally, abnormal findings are not always directly related to the pain a person is feeling. A patient with severe knee pain may have an MRI that reveals no abnormalities, or a patient with acute but mild back pain will have an MRI showing severe degenerative changes of their discs and two herniated discs.
In particular, non-coordinated findings can be very frustrating for a patient and leave them feeling confused as to the next best step to take. To make matters even more confusing, the literature indicates that positive imaging findings are common and may not be the best guide for future care decisions. A 2020 study performed by Horga et al on 115 asymptomatic (without any pain) adults revealed that 97% showed abnormalities in their knee MRIs. These findings included meniscal tears (30%), cartilage abnormalities of the patellofemoral joint (57%), and moderate tendon lesions (21%).
Similar findings are present in low back pain: Brinjikhi et al performed a systematic review gathering information about positive low back imaging findings on asymptomatic adults. Data gathered on over 3,000 people revealed that by age 20, there was a 27% prevalence of degenerative disc findings and by age 50, that number rose to 80%. According to their findings, it is more common to have degenerative changes beginning at age 30 than to not – and this was in an entire population of people without back pain!
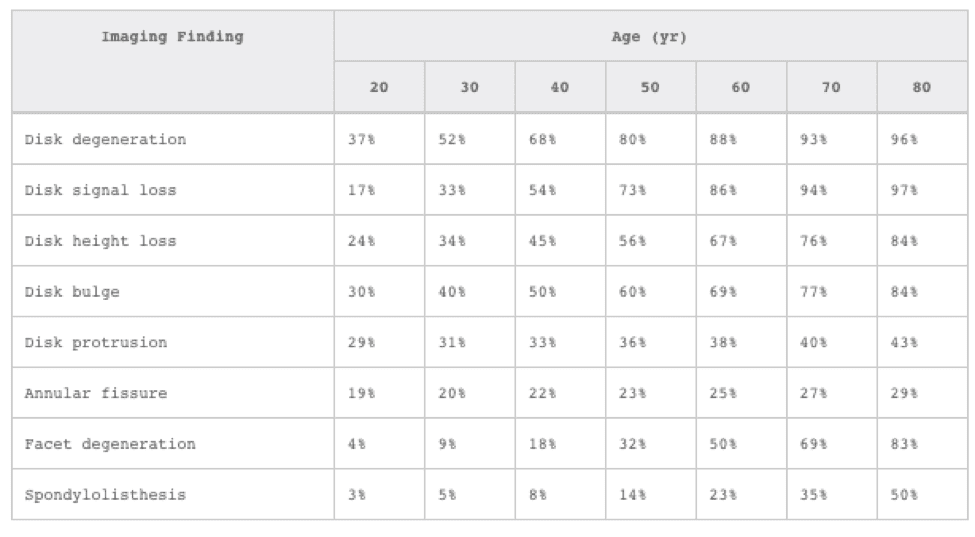
Prevalence of abnormal MRI findings in the lower back for 3,110 asymptomatic individuals (Brinkikji et al).
It is important to understand that imaging has its place in healthcare and can be very helpful and necessary in certain situations. The American College of Physicians and the American Pain Society published a joint clinic practice guideline regarding the diagnosis and management of low back pain in 2007.
According to this guideline, clinicians should perform diagnostic imaging only if they detect severe or progressive neurologic deficits, suspect serious underlying pathology, or identify the patient as a potential candidate for surgery or epidural steroid injections. The guidelines also suggest that clinicians should not perform imaging for patients with nonspecific low back pain.
In summary, imaging helps rule out serious pathology, provides diagnostic clarity when surgical intervention is necessary, and guides physicians in administering epidural steroid injections. Routine use of imaging, however, may be causing more fear, more confusion, and more cost than necessary.
If you are confused about your recent imaging findings or have pain but are unsure if you need imaging in the first place, stop by Lakeshore Physical Therapy to discuss it with one of our experienced therapists. Additionally, we offer complimentary injury screens to decide what is the right next step for you. We want you to feel confident in your healthcare decisions and clear on your road to recovery!
References:
Brinjikji, P.H. Luetmer, B. Comstock, B.W. Bresnahan, L.E. Chen, R.A. Deyo, S. Halabi, J.A. Turner, A.L. Avins, K. James, J.T. Wald, D.F. Kallmes and J.G. Jarvik, Systematic Liertaure Review of Imaging Features of Spinal Degeneration in Asymptomic Populations. American Journal of Neuroradiology. April 2015, 36 (4) 811-816
Flynn, T.W., Smith, B., Chou, R. Appropriate Use of Diagnostic Imaging in Low Back Pain: A Reminder That Unnecessary Imaging May Do as Much Harm as Good. Journal of Orthopedic and Sports Medicine. Nov 2011, 41 (11) 838 – 846.
Horga, L.M., Hirschmann, A.C., Henckel, J. et al. Prevalence of abnormal findings in 230 knees of asymptomatic adults using 3.0 T MRI. Skeletal Radiol (2020).
Lewis, J.S., Cook, C.E, Hoffman, T.C., O’Sullivan, P., The Elephant in the Room: Too Much Medicine in Musculoskeletal Practice. Journal of Orthopedic and Sports Medicine. Jan 2020, 50 (1) 1-4.
